Why is Inclusivity Crucial in Prenatal & Postpartum Care?
Folks often bring up how everyone’s pregnancy is unique; that no pregnancy is the
same as any other. What is not often discussed is how being part of a social minority or
having an intersectional life experience can turn this sense of uniqueness into an
overwhelming form of isolation.
In this post, I discuss the concept of social categories/intersectionality and how
inclusion in doula care can make all the difference for these individuals.
What is Intersectionality?
You may have noticed how our society uses social categorization to determine how
to treat individuals. These categories include but are not limited to: Ethnicity, Race,
Religion, Gender & Sexuality, Neurological Makeup, Socioeconomic & Marital Status.
When these categories overlap one another in a person’s life experience, this is what is
considered intersectionality.
An example of this is when a person is part of an ethnic minority as well as being
gay. This person will face obstacles and discriminations from each of these overlapping
social categories. They will face more complex difficulties interacting with the world
compared to an individual who is Caucasian(white) and gay, or an individual who is from
an ethnic minority and heterosexual. It is also common for more than two categories to
overlap, which creates more stigma with each intersectional layer.
Question: Have you ever considered how intersectionality has affected your
prenatal/postpartum experience, or the experience of someone you cherish?
Why Should Inclusivity be Considered in Prenatal/Postpartum Care?
When someone is considering or is in the motion of pregnancy, they are
experiencing a monumental transition in their life. Pregnant individuals have many
emotional landmines to combat during this time, such as financial strain and the potential
of complications during labor. These concerns are discussed frequently in prenatal care
and postpartum support groups. Though these communities are remarkable for creating a
sense of belonging, they usually only pertain to the experiences of
cis, heterosexual, Caucasian women.
What is less known is that individuals from a social categorical minority face many
forms of discrimination – such as structural and interpersonal - when going through their
pregnancy journey. Discrimination is even more labyrinthian when an individual with an
intersectional life experience faces pregnancy. This is precisely why we should promote
understanding of intersectionality and inclusion of all social categorical minorities.
Question: Have you or anyone you know faced discrimination during
prenatal/postpartum care? What support should have been accessible to ease
stress on your journey?
What Does Inclusivity Look Like in Doula Care?
If you have ever been supported by a doula during prenatal/postpartum, you may
know that the doula’s goal is to support you during your pregnancy journey. They provide
you with prenatal information and guidance.
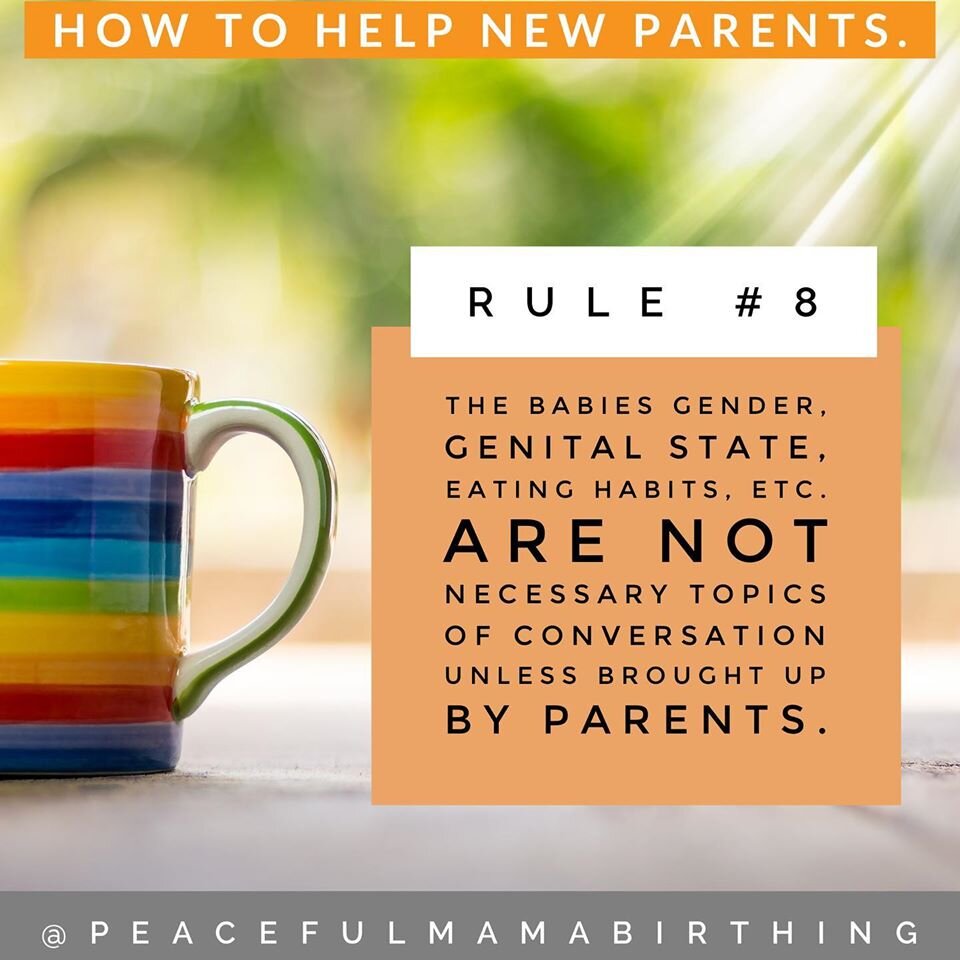
Further yet, a genuine doula is there to promote your voice. As a parent-to-be it is
essential for you to be able to make informed decisions. Your doula should listen and
encourage you to choose your personal choices for pregnancy/labor, promoting self-
empowerment.
When these fundamental skills are paired with inclusivity, a doula can provide a full
range of support to individuals who never thought pregnancy or parenthood was possible
in their experience. The emotional and informational support that doulas provide must be
made accessible to those doting parents who have been combating societal expectations
at every turn.
Question: Have you or someone close to you received doula care that made you
feel heard? How would it have affected you if you didn’t have access to this support
due to your personal identity?
Conclusion
Though everyone’s journey through pregnancy is unique, there are those who face
more obstacles to supportive care and prenatal/postpartum education. Those from social
categorical minorities or with intersectional life experiences may face more adversity whennavigating childbirth and parenthood. Common forms of care and support may not even be
available to them.
The more birth care services (such a doula care) and medical facilities educate their
staff about intersectionality and inclusion; the less likely potential doting parents will be
left out of the conversation.
I encourage whoever is reading this to reflect on how inclusivity has presented itself
in your prenatal/postpartum experience, or how the lack of inclusivity has affected your
journey.
If you are comfortable answering any of the provided in each section above, we at
Peaceful Birth Company would love to hear your thoughts/stories. Stay peaceful.
Kit Nave (Intern)
10/27/2025